Table Of Contents
- WHAT ARE FAR-UVC LIGHTS?
- UV LIGHT THAT IS SAFE FOR HUMANS BUT BAD FOR BACTERIA AND VIRUSES
Listen to the article
What are far-UVC lights?
How effective are far-UVC lights in sanitizing bacteria and germs-infected everyday items? Health-acquired Infection (HAI). A person who gets contamination while getting care in the emergency clinic will probably require a more extended remain, extravagant for the social insurance framework. In the most pessimistic scenario, they become genuinely sick and kick the bucket. The Center for Disease Control reports that human services obtained contaminations execute around 100,000 individuals consistently in the US.
We need some new plans to manage HAIs, yet which diseases explicitly? This wide range of diseases can incorporate complexities from a medical procedure or a non-clean instrument, an absence of handwashing, or experience with messy surfaces. We should see one restricted subset of these contaminations, Clostridium Difficile, which most ordinarily influences more established grown-ups in emergency clinics or long haul care offices. These diseases can emerge out of loose bowels. It aerosolizes, the microscopic organisms land on a surface, colonize, somebody reaches that surface, gets in their body, and is debilitated.
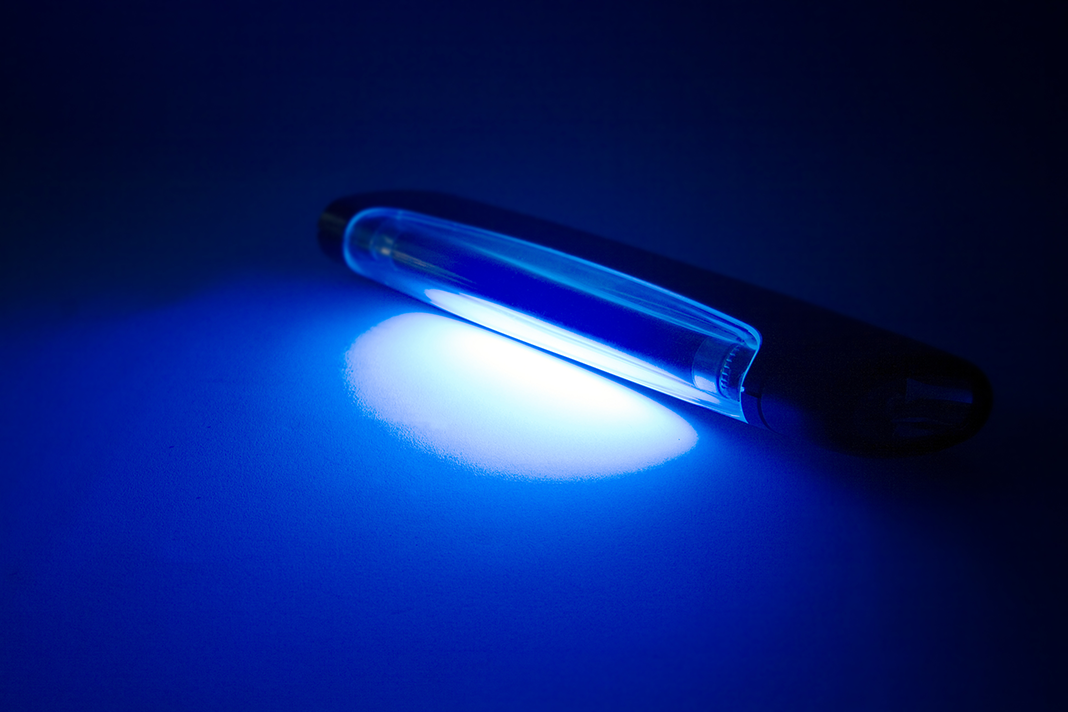
Here’s the place the lights come in: Ultraviolet Germicidal Irradiation utilizing Ultraviolet C (shortwave bright light) lighting, or UVc, for short has incredible potential. The utilization of UVc has entrenched in the water treatment industry; however, its usage in human services isn’t yet across the board. UVc lights should use to eliminate germs in the medical clinic, water supplies, air taking care of gear, and clean gadget handling. In any case, the use of an UVc lighting framework in shared washrooms to illuminate C. diff germs after the toilet has been utilized despite everything has all the earmarks of being the particular case, rather than the standard.
A third zone to consider is versatile electronic gadgets. In the present “shrewd medical clinics,” specialists and human services colleagues are consistently utilizing mobile phones, tablets, or COWS (PCs on wheels) as they get out and about. Studies show that these gadgets, particularly PDAs, are probably going to be tainted.
We could never suggest that UV light be the primary type of room cleaning; however, in a time of expanding anti-microbial obstruction, it could turn into a significant expansion to clinics’ arms stockpiles.
UV LIGHT THAT IS SAFE FOR HUMANS BUT BAD FOR BACTERIA AND VIRUSES
Researchers are ceaselessly on the chase for new weapons that explicitly target pathogenic organisms in the consistent fight against the spread of irresistible infections. Presently, specialists from the Center for Radiological Research at Columbia University Irving Medical Center (CUIMC) accept they may have discovered another, minimal effort answer for destroying airborne infections in indoor open spaces.
The exploration group found that consistent low dosages of far bright C (far-UVC lights) light can execute airborne influenza infections without hurting human tissues. The discoveries from the new examination—distributed today in Scientific Reports in an article entitled “Far-UVC Lights: A New Tool to Control the Spread of Airborne-Mediated Microbial Diseases”— proposes that utilization of overhead far-UVC lights in emergency clinics, specialists’ workplaces, schools, air terminals, planes, and other open spaces could give an incredible beware of occasional flu plagues, just as flu pandemics.“Sadly, ordinary germicidal UV light is additionally a human wellbeing risk and can prompt skin malignant growth and waterfalls, which forestalls its utilization out in the open spaces,” clarified senior examination specialist David Brenner, Ph.D., head of the Center for Radiological Research and educator at CUIMC.
Brenner and his associates conjectured that a tight range of bright light called far-UVC lights could slaughter microorganisms without harming solid tissue. Additionally, the specialists exhibited that far-UVC lights were powerful at murdering MRSA (methicillin-safe Staphylococcus aureus) microorganisms, a typical reason for careful injury diseases, yet without hurting human or mouse skin.
“Far-UVC lights have a constrained range and can’t enter through the external dead-cell layer of human skin or the tear layer in the eye, so it is anything but a human wellbeing danger,” Brenner noted. “But since infections and microscopic organisms are a lot littler than human cells, far-UVC lights can arrive at their DNA and execute them.”In this investigation, aerosolized H1N1 infection—a typical strain of influenza infection—was delivered into a test chamber and presented to exceptionally low portions of 222-nm far-UVC light. A benchmark group of aerosolized infection has been given to the UVC light. The far-UVC light deactivated the influenza infections, with about a similar effectiveness as traditional germicidal UV light.
“We show just because that far-UVC productively inactivates airborne aerosolized infections, with an extremely low portion of 2 mJ/cm2 of 222-nm light inactivating >95% of aerosolized H1N1 flu infection,” the creators composed. “Persistent exceptionally low portion rate far-UVC light in indoor open areas is a promising, protected, and cheap device to lessen the spread of airborne-intervened microbial illnesses.”
At the cost of under $1000 per light—a price that would decline if the lights were mass delivered—far-UVC lights are moderately cheap. It could permit the apparatus to use unmistakably. A more significant number of spots than UV lights had utilized, prompting conceivably broad clearing impacts toward reducing the spread of numerous irresistible microbes.
“If our outcomes are affirmed in different settings, it follows that the utilization of overhead low-level far-UVC light in open areas would be a protected and productive technique for restricting the transmission and spread of airborne-intervened microbial sicknesses, for example, flu and tuberculosis,” Dr. Brenner closed.